Urgent care centers operate in a fast-paced environment where patients expect quick treatment, transparent pricing, and efficient service. Behind this rapid workflow is a complex financial and administrative process that requires immediate attention. This is where urgent care billing comes into play. High-quality urgent care billing services ensure accurate documentation, clean claim submissions, correct urgent care CPT coding, and stronger reimbursement outcomes. As patient traffic continues to rise, **[Urgent Care RCM](https://asprcmsolutions.com/specialities/urgent-care-rcm)** (Revenue Cycle Management) becomes essential for smooth operations.
Urgent care centers face unique billing challenges due to walk-in visits, multiple payer types, varied procedures, and documentation gaps. To maintain strong cash flow, every clinic needs a well-structured billing workflow supported by a modern urgent care EHR system combined with specialized coding and claim management.
Why Urgent Care Billing Matters
Urgent care clinics deal with high patient volume. Even small coding or claim errors can create delays, denials, and revenue leakage. Accurate urgent care billing ensures:
Faster payments
Increased clean claim rate
Precise charge capture
Proper urgent care CPT coding
Better compliance with payer rules
Stronger financial outcomes
Without a solid Urgent Care RCM system, clinics may experience operational inefficiency, claim backlogs, and reduced profitability.
Key Challenges in Urgent Care Billing
Urgent care clinics handle a wide variety of services such as X-rays, wound care, injections, fracture treatments, flu tests, and minor procedures. These services require accurate coding and documentation.
1. High patient volume
Walk-in visits create unpredictable patient load. Billing teams must process claims quickly to maintain consistent cash flow.
2. Wide range of CPT codes
Urgent care CPT coding covers evaluation visits, diagnostic tests, injury care, and procedures. Incorrect code selection affects payment.
3. Multiple payer types
Urgent care bills:
Commercial insurance
Medicare
Medicaid
Workers’ compensation
Self-pay
Each payer has different rules, creating complexity in Urgent Care Revenue Cycle Management.
4. Documentation gaps
If clinicians do not document symptoms, exam findings, imaging impressions, or treatments clearly, claims may get denied.
5. Prior authorization issues
Some payers need approvals for tests or procedures, which can delay claim processing.
Urgent Care RCM: Foundation for Sustainable Clinic Operations
Urgent Care RCM covers the entire financial lifecycle of a patient visit. A strong RCM structure ensures that every step—from patient check-in to final payment—is efficient, accurate, and fully compliant.
Key components of Urgent Care RCM include:
1. Front desk verification
Insurance eligibility
Co-pay collection
Demographics accuracy
Accurate intake prevents denied claims later.
2. Charge capture
Every service must be documented to avoid revenue loss.
3. Urgent care CPT coding
Certified coders review charts and apply the correct CPT, ICD-10, and HCPCS codes.
4. Claim submission
Clean claim submission ensures faster reimbursement.
5. Denial management
Quick resolution of coding- and documentation-related denials improves cash flow.
6. Patient billing
Transparent patient statements reduce confusion and improve collection rates.
Strong RCM processes help urgent care centers maintain financial stability even during peak seasons like flu outbreaks or travel surges.
Role of Urgent Care EHR in Billing Accuracy
An urgent care EHR system streamlines workflow by connecting clinical documentation, coding, and billing operations. A good EHR should support:
Real-time documentation
Automatic charge capture
Built-in templates for common urgent care services
Seamless integration with billing software
Easy-to-use provider notes
When urgent care EHR is optimized, coding accuracy improves significantly. This reduces errors, increases clean claims, and helps clinics maintain strong revenue cycles.
Urgent Care CPT Coding: Ensuring Accurate Reimbursement
Correct urgent care CPT coding is vital for capturing the full value of services provided. Common codes include:
Evaluation & Management codes for new and established patients
Procedure codes for sutures, abscess drainage, nebulizer treatments, etc.
Diagnostic test codes such as COVID tests, strep tests, urinalysis, ECGs, X-rays
Mistakes in urgent care CPT coding result in underpayment or claim rejection. Certified coders ensure:
Proper code selection
Correct modifier use
Compliance with payer guidelines
Accurate linking of diagnoses and procedures
Coders also verify documentation to ensure it supports the level of service billed.
Benefits of Outsourced Urgent Care Billing Services
Many clinics choose outsourced urgent care billing services to handle their coding and claim processing. Outsourcing provides:
1. Higher accuracy
Certified coders specialize in urgent care coding requirements.
2. Faster turnaround
Claims are processed quickly, improving cash flow.
3. Reduced administrative burden
Clinic staff can focus on patient care.
4. Better denial control
Billing teams track patterns and resolve issues efficiently.
5. Increased revenue
Every charge is captured and coded correctly.
6. Access to experts
Specialized billing teams bring deep knowledge of payer rules, urgent care EHR systems, and Urgent Care Revenue Cycle Management best practices.
How Strong Billing Improves Urgent Care Profitability
High-performing urgent care billing services prevent revenue leakage by:
Ensuring complete documentation
Applying correct CPT codes
Submitting clean claims
Reviewing coding-related denials
Performing regular internal audits
Tracking KPIs like first-pass acceptance rate
A well-optimized system can increase revenue by reducing coding errors, improving claim approval rates, and enhancing the accuracy of urgent care CPT coding.
Technology Trends Transforming Urgent Care Billing
Urgent care billing continues to evolve with modern digital tools. Key tools include:
AI-assisted coding
Automated claim scrubbing
EHR-integrated charge capture
Real-time denial analytics
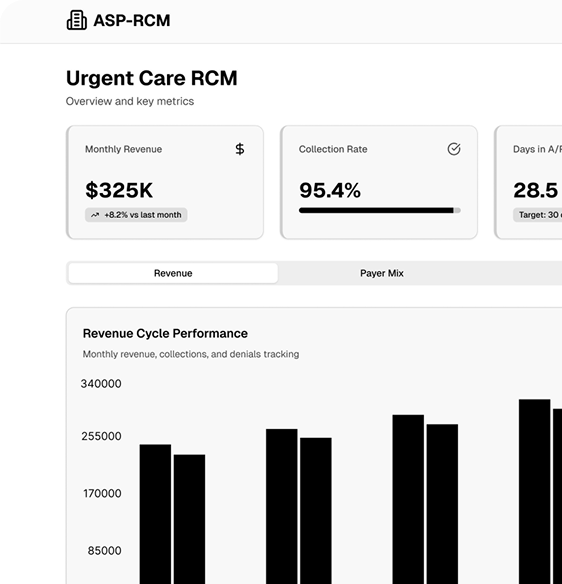
Predictive financial dashboards
These tools improve accuracy, reduce manual effort, and support better decision-making.
Conclusion
Urgent care centers need efficient, accurate, and scalable billing processes to maintain financial stability. Urgent care billing services, combined with strong Urgent Care RCM and modern urgent care EHR systems, ensure clean claim submissions, correct urgent care CPT coding, and improved reimbursement. With rising patient volume and increasing payer complexity, professional billing support helps urgent care clinics maintain operational speed, financial strength, and high-quality patient care.